Opioid Use During Pregnancy
 Untreated opioid use disorder during pregnancy can have devastating consequences for the unborn baby.
Untreated opioid use disorder during pregnancy can have devastating consequences for the unborn baby.
Fluctuating levels of opioids in the mother may expose the fetus to repeated periods of withdrawal, which can harm placenta function.
Other direct physical risks include:
- neonatal abstinence syndrome
- stunted growth
- preterm labor
- fetal convulsions
- fetal death
Other indirect risks to the fetus include:
- increased risk for maternal infection (e.g., HIV, HBV, HCV)
- malnutrition and poor prenatal care3
- dangers from drug seeking (e.g., violence and incarceration)
What is Neonatal Abstinence Syndrome?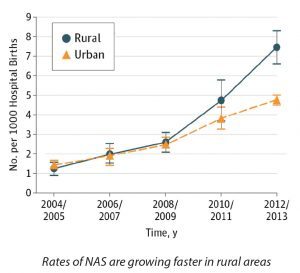
Neonatal abstinence syndrome (NAS) occurs when an infant becomes dependent on opioids or other drugs used by the mother during pregnancy. The infant experiences withdrawal symptoms that can include (but are not limited to) tremors, diarrhea, fever, irritability, seizures, and difficulty feeding.
NAS increased nearly fivefold nationally between 2000 to 2012,6,7 coinciding with rising rates of opioid prescribing to pregnant women.
Science Driven Solutions
Evidence-Based Treatment
Buprenorphine and methadone have both been shown to be safe and effective treatments for opioid use disorder during pregnancy. While NAS may still occur in babies whose mothers received these medications, it is less severe than in the absence of treatment. Research does not support reducing medication dose to prevent NAS, as it may lead to increased illicit drug use, resulting in greater risk to the fetus.
Methadone vs. Buprenorphine
A recent meta-analysis showed that methadone is associated with higher treatment retention. However, buprenorphine resulted in:
- 10 percent lower incidence of NAS
- decreased neonatal treatment time by 8.46 days
- less morphine needed for NAS treatment by 3.6mg
Patients should work with their doctor to determine which medication is best for them.
Breastfeeding During Treatment
Although breastfeeding is typically low among mothers with opioid use disorder, studies have found that breastfeeding can reduce length of hospital stay and need for morphine treatment in infants. Unless there are specific medical concerns (e.g., maternal HIV infection), encouraging mothers to breastfeed and swaddle newborns may ease infant NAS symptoms and improve bonding.
Methadone and Buprenorphine Can Effectively Treat Opioid Use Disorder During Pregnancy
Methadone has been used to treat pregnant women with opioid use disorder since the 1970s and was recognized as the standard of care by 1998. Since then, studies have shown that buprenorphine is also an effective treatment option. The American College of Obstetricians and Gynecologists and the American Society of Addiction Medicine support methadone and buprenorphine treatment as best practice for opioid use disorder during pregnancy.
Benefits of Treatment During Pregnancy. Treatment with methadone or buprenorphine improves infant outcomes by:
- stabilizing fetal levels of opioids, reducing repeated prenatal withdrawal
- linking mothers to treatment for infectious diseases (e.g., HIV, HBV, HCV), reducing likelihood of transmittal to the unborn baby
- providing opportunity for better prenatal care
- improving long-term health outcomes for the mother and baby
Compared to untreated pregnant women, women treated with methadone or buprenorphine had infants with:
- lower risk of NAS
- less severe NAS
- shorter treatment time
- higher gestational age, weight, and head circumference at birth
Solutions Driven Science
Increasing Treatment Prescribing
NIDA-funded studies are evaluating key barriers and facilitators to prescribing methadone and buprenorphine for pregnant women. Current projects include:
- validating reliable screening tools to identify pregnant women in need of treatment
- analyzing infant outcomes to inform medication selection for opioid use disorder during pregnancy
- evaluating behavioral interventions for opioid misuse in pregnancy
Improving Treatment Strategies
Treatment with methadone or buprenorphine does pose some risk for NAS. Divided dosing with methadone—taking smaller doses more often—reduces fetal exposure to withdrawal periods. Mothers treated with divided doses of methadone have babies with lower NAS severity. Currently, an NIH-funded study is examining buprenorphine during pregnancy and how to improve buprenorphine dosing regimens.
Improving Engagement in Treatment
- Stigma and bias among healthcare providers can result in both under-reporting of drug use and insufficient medication dosing, which often lead to delayed or ineffective treatments.
- Eighteen states classify maternal drug use as child abuse, and three states consider it as reason for involuntary hospitalization, disincentivizing women from seeking treatment.
- Women who are allowed to stay with their children during treatment are more likely to start treatment and maintain abstinence.
Supporting access to treatment. Health insurance providers that cover treatment for substance use disorders are required to provide coverage equivalent to what is provided for other health conditions.